Testosterone Lab Testing
The Measurement Of Testosterone
Roland R. Tremblay
Learning Objectives
1. To understand that andropause is constituted by two structural levels and that the surface structure is amenable to diagnosis and treatment.
2. To learn that although the measurement of total testosterone (TT) in blood is still useful for the diagnosis of hypogonadism in men, in the aging male, TT may be a misleading measure of true gonadal function.
3. To develop a better understanding of the complementary role of calculated free testosterone measurements as an index of androgenicity in aging men, and to realize that these indices do not convey any information about androgen receptors and enzymes inside target cells.
4. To understand that testosterone indices are reliable to a limited extent, as illustrated with bioavailable testosterone (bio-T), given the uncertainty as to whether the dissociation of the specific steroid-SHBG complex is partial or complete at the cellular level, and given the controversy about the possible androgenic activity of the SHBG-testosterone fraction itself.
Introduction
As opposed to metabolic disorders, such as diabetes mellitus and hyperthyroidism due to Graves’ disease, which are associated with an elevation of either blood glucose or thyroid hormones, the multifactorial clinical entity of andropause appears to be due to a progressive decline in androgen levels with advancing age. In the coming years, however, this vision of andropause may be considered a simplistic explanation of an imbalance between anabolic and catabolic factors that characterize aging. As reported by Tremblay, 1 andropause is constituted by two structural levels: a “deep-structure” that requires long-term research and a “surface structure” (hypogonadism) that can be accessed now by physicians. In the short term, worldwide efforts should be coordinated towards enriching the knowledge of this “surface structure”, while at the same time supporting research that will define this entity unambiguously in order that treatment can be undertaken with confidence and with complete awareness of any potential side-effects.
Since our current state of knowledge indicates that male hypogonadism is the major determinant of andropause, it is reasonable that the focus of our biological testing is on assessing the physiological changes that occur as gonadal function changes with advancing age. Changes that indicate testosterone deficiency include cognitive and sexual dysfunctions, decrease in muscle mass, development of osteoporosis and increase in fat mass. 2 In hypopituitarism, for which there are more than 12 underlying causes (N=1014 patients), multiple regression analyses have confirmed an association between testosterone therapy and reduced mortality in both sexes. 3 Androgens may also be an important factor for maintenance of skeletal health in women with hypopituitarism. 4
Testosterone Measurement in Blood
Aging is associated with decreases in total, free and bioavailable testosterone concentrations in serum, as well as with an elevated sex hormone binding globulin (SHBG) level leading to increased serum SHBG testosterone binding in the circulation and a decreased metabolic clearance rate of testosterone. 5
Physicians are often uncertain about which measure of testosterone best reflects hypogonadism and how to use and interpret the tests of testosterone concentration that are available.
Total Testosterone (TT)
TT is a combination of circulating testosterone bound to carrier proteins (albumin, SHBG, transcortin, transferrin) and the free/unbound hormone. The measurement of TT was achieved formerly by double isotope techniques for research purposes and elucidation of difficult clinical diagnoses such as male or female pseudohermaphroditism, congenital adrenal hyperplasia and the androgen insensitivity syndrome.
One week of laboratory work was required to perform 12 TT measurements by the older technique. TT can now be measured by a routine and inexpensive assay for the assessment of sexual dysfunction, mood disorders, chronic fatigue syndrome, male infertility, female hirsutism, menopausal women and andropause, but with a relatively low diagnostic yield. Most laboratories that measure TT make use of commercially available kits Table 1, which have a high degree of variability and inaccuracy. 6
Until now, many commercial kits for the measurement of TT have been of limited value in confirming clinical studies suggestive of either partial androgen privation or androgen excess. The main concerns about these assays are purely technical:
1) the protein-labelling of testosterone (antigen);
2)the source of the antibodies developed in small mammals;
3) the specificity of the various antibodies;
4) the usage of one or two antibodies;
5) the unextracted testosterone from its biological milieu.
Technical difficulties are amplified by physicians who expect too much from the test and by biochemists who do not have the opportunity to validate the assay with a sufficient number of normal individuals. In general, however, all testosterone assays can confirm the diagnosis of castration in males and in females and of a testosterone secreting ovarian or adrenal tumor in a young woman with severe hirsutism and virilizaton.
Bioavailable Testosterone (Bio-T)
Aging is associated with pituitary and hypothalamic senescence, with a decreased synthesis of androgens by the Leydig cells in the testes and the zona reticularis of the adrenal cortex, and finally with an increased hepatic production of SHBG. Several factors thus prevail favouring a new state of equilibrium between bound and free hormones in blood. The measurement of free hormones is best achieved by equilibrium dialysis. This gold standard is used primarily in research protocols and, generally speaking, a fairly good agreement has been observed between male free hormones and androgenicity when no disorders such as androgen receptor insensitivity or polymorphism are involved in the pathogenesis of either phenotypic abnormalities or infertility problems.
Since specific assays for the direct measurement of free testosterone (FT) in serum are unreliable 7 and equilibrium dialysis is not feasible on a routine basis, bioavailable testosterone (bio-T) is now considered the silver standard by many clinicians. Bio-T corresponds to the combination of serum free and albumin-bound testosterone. This concept is based on in vitro kinetic calculations (dissociation of T from albumin around 1 second as opposed to a dissociation of T from SHBG of 20-second magnitude); however, the basic assumption that T becomes completely free during the capillary transit of the hormone, and hence available to cytoplasmic androgen receptors, has been challenged by some authors.
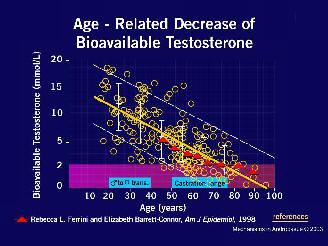
Andropausal symptoms are associated with bio-T values lower than 2.5-3.0 nmol in 15-20% of aged man who believe that the quality of their life is threatened by these symptoms. Unfortunately, despite the availability of several questionnaires, there are none which clearly identify andropause as a unique entity, and as a consequence there is no strong correlation between any andropause questionnaire and bio-T values. Bio-T remains, however, a convenient marker of androgen status and is most strongly related to diseases and risk factors such as osteopenia and mood disorders in aged individuals. The merits of this assay are summarized in Table 2 and Table 2b.
Free Testosterone (FT)
The purpose of FT measurement is to correct the total testosterone concentration for the effect of variable binding by SHBG. It would appear, therefore, to be more appropriate to measure FT rather than TT when investigating for hypoandrogenicity. Methods available to measure FT can be complex (equilibrium dialysis and calculated free testosterone (CFT)) or simple (the commercial FT kit “Coat-A-Count” using an analog tracer). 11
What is easy, however, does not necessarily serve the best interests of patients, because analog tracers do, in fact, bind to serum proteins leading to diagnostic unreliability, 12 more specifically to underestimation of FT in serum. Surprisingly, nearly 50% of authors around the world are still publishing research results in endocrine journals based on an unreliable, but easy to use assay. 13
The new trend since the publications of Vermeulen et al. in 1999, Tremblay in 2001 and Morley et al. in 2002,14 favors the simultaneous measurement of TT and SHBG (e.g Irma-Count, DPC) and then a calculated free testosterone (CFT) value derived from the law of mass action at equilibrium using a specially designed computer program containing a complex mathematical formulation. The program was supplied to us by Dr. J.M. Kaufman, Ghent, Belgium. The above-mentioned three authors reached a similar conclusion when bio-T was compared to CFT (Figure 2). There is an excellent correlation between bio-T measurements and CFT with “r” values ranging between 0.7 and 0.9. Table 3 and Table 3b summarizes a few issues (pro and con) to take into account when using CFT.
Key Points
1. Laboratories able to provide a CFT value as an index of androgenicity should use commercial kits similar to those selected by Vermeulen, Tremblay and Morley in order to reproduce published results. Validation of the CFT measurement should be performed by each laboratory using this technique with populations of young adults and older men in good health. 15
2. Many laboratories keep serum specimens for 2 to 3 weeks at –20°C. During that time no significant changes occur in the T and SHBG kinetics. This sample can be frequently used to add other tests, as needed, or if not originally ordered.
Conclusion
Aging men with symptoms of hypogonadism share clinical manifestations very similar to those of younger individuals distressed by pituitary tumors, selective gonadotropin insufficiency and testicular failure of various origins. The clinical diagnosis in the latter conditions may, indeed, be supported by TT measurements; however, in situations such as aging, thyroid disorders, obesity and the use of certain medications (anti-androgens, anti-epileptic agents, estrogens, progestational agents), the correlation between the clinical symptoms and TT concentration is often poor. This observation could be associated with abnormal kinetics between T and SHBG or ascribed to variations in SHBG concentrations during life and in the course of several chronic illness. 16 The best method of assessing hypoandrogenicity is to measure bio-T or CFT to minimize the number of false positive or false negative associations between the clinical state and testosterone indexes. 14
References
1. Tremblay RR. Practical consequences of the validation of a mathematical model in assessment of partial androgen deficiency in the aging male using bioavailable testosterone. The Aging Male 2001;4:23-9.
2. Bhasin S, Buckwalter JG. Testosterone supplementation in older men: A rational idea whose time has not yet come. J Androll 2001;22:718-31.
3. Tomlinson JW, Holden N, Hills RK, Wheatley K, Clayton RN, Bates AS, Sheppard MC, Stewart PM. Association between premature mortality and hypopituitarism. Lancet 2001;357:425-31.
4. Miller KK, Biller BM, Hier J, Arena E, Klibanski A. Androgens and bone density in women with hypopituitarism. J Clin Endocrinol Metab 2002;87:2770-6.
5. Kandeel FR, Koussa VK, Swerdloff RS. Male sexual function and its disorders: Physiology, pathophysiology, clinical investigation, and treatment. Endocr Rev 2001;22:342-88.
6. Boots LR, Potter S, Potter D, Azziz R. Measurement of total serum testosterone levels using commercially available kits: High degree of between-kit variability. Fertil Steril 1998;69:286-92.
7. Rosner W. Errors in the measurement of plasma free testosterone. J Clin Endocrinol Metab 1997;82:2014-5.
8. Vermeulen A, Verdonck L, Kaufman JM. A critical evaluation of simple methods for the estimation of free testosterone in serum. J Clin Endocrinol Metab 1999;84:3666-72.
9. Tremblay RR, Dubé JY. Plasma concentrations of free and non-TeBG bound testosterone in women on oral contraceptives. Contraception 1974;10:599-605.
10. Tremblay RR. Un nouvel outil diagnostique pour l’andropause. Le Clinicien 2001;16:158-68.
11. Wilke TJ, Utley DJ. Total testosterone, free-androgen index, calculated free testosterone, and free testosterone by analog RIA compared in hirsute women and in otherwise-normal women with altered binding of sex-hormone binding globulin. Clin Chem 1987;33:1372-5.
12. Winters SJ, Kelley DE, Goodpaster B. The analog free testosterone assay: Are the results in men clinically useful? Clin Chem 1998;44:2178-82.
13. Rosner W. An extraordinarily inaccurate assay for free testosterone is still with us. J Clin Endocrinol Metab 2001;86:2903.
14. Morley JE, Patrick P, Perry HM 3rd. Evaluation of assays available to measure free testosterone. Metabolism 2002;51:554-9.
15. Emadi-Konjin P, Bain J, Bromberg IL. Evaluation of an algorithm for calculation of serum “bioavailable” testosterone (BAT). Clin Bioch 2003 (accepted for publication).
16. Turner HE, Wass JA. Gonadal function in men with chronic illness. Clin Endocrinol 1997;47:379-403.







